Addressing Youth Loneliness and Social Disconnection Through Community-Based Public Health Interventions
Abstract
Youth loneliness and social disconnection have emerged as critical public health concerns, with significant implications for adolescent mental health, academic engagement, and long-term well-being. Middle and high school students from underrepresented communities experience heightened vulnerability due to social determinants of health, limited access to mental health resources, and structural inequities. This study examines a community-based public health practicum initiative designed to assess and address youth loneliness through mixed-methods needs assessment and intervention planning. Quantitative survey data and qualitative stakeholder input revealed elevated levels of perceived loneliness, low awareness of mental health resources, and significant barriers to help-seeking among youth. Findings underscore the importance of culturally responsive, community-centered interventions that prioritize social connection as a protective factor.
Keywords: youth loneliness, social disconnection, adolescent mental health, social determinants of health
Introduction
Loneliness and social disconnection among adolescents have gained increasing attention as population-level public health issues, particularly because social connection functions as a protective factor for mental and physical well-being across the life course (Office of the U.S. Surgeon General, 2023). Adolescence is a critical developmental period for forming and practicing social bonds; however, many youth report persistent feelings of isolation that co-occur with anxiety, depressive symptoms, and reduced academic engagement (Loades et al., 2020). National surveillance data further reflect the broader context in which these concerns are unfolding, with a substantial proportion of U.S. high school students reporting poor mental health indicators in recent years (Centers for Disease Control and Prevention [CDC], 2024). Importantly, loneliness is not only an individual experience it is shaped by social determinants of health, including access to supportive relationships, safe community spaces, culturally responsive resources, and school connectedness (Office of the U.S. Surgeon General, 2023). These concerns have intensified alongside shifts in how adolescents socialize, including increased reliance on digital communication and reduced in-person interaction in the wake of COVID-19 disruptions (Loades et al., 2020). Research on technology use suggests that greater screen-based engagement may be associated with lower psychological well-being and social functioning for some youth, although the strength and mechanisms of this relationship can vary across individuals and contexts (Twenge & Campbell, 2018). Taken together, the evidence supports framing youth loneliness as a public health issue requiring community-based, prevention-oriented strategies that strengthen protective relationships and expand access to supportive resources (CDC, 2024; Office of the U.S. Surgeon General, 2023).
Research Question
How does social disconnection affect adolescents’ mental well-being, and how can community-based public health interventions reduce loneliness and improve access to supportive resources among underrepresented youth?
Methods
This study employed a mixed-methods, community-based needs assessment design conducted as part of a Master of Public Health practicum in partnership with a youth- serving community health organization. A mixed-methods approach was selected to capture both the magnitude of youth loneliness and social disconnection and the contextual factors shaping these experiences within the community. Mixed-methods designs are particularly well suited for public health practice because they allow researchers to integrate numerical trends with lived experiences, thereby producing findings that are both empirically grounded and practically actionable (Creswell & Plano Clark, 2018).
Quantitative and qualitative methods were intentionally combined to strengthen the validity and usefulness of the assessment. Quantitative data provided measurable indicators of prevalence, patterns, and disparities related to loneliness, social connectedness, and access to mental health resources. Qualitative stakeholder input complemented these findings by offering deeper insight into cultural norms, structural barriers, and service gaps that influence youth experiences but are not easily captured through surveys alone (Palinkas et al., 2011).
The community-based orientation of the needs assessment emphasized collaboration with local partners throughout the research process, including instrument development, data interpretation, and application of findings. Community-engaged approaches are recommended in public health practice to ensure cultural relevance, enhance trust, and increase the likelihood that results will translate into sustainable interventions (Israel et al., 2010). By situating the assessment within a practicum setting, this study intentionally bridged public health research and applied practice, allowing findings to directly inform program planning, intervention development, and organizational capacity building.
Results
Quantitative findings indicated moderate to high levels of perceived loneliness among a substantial proportion of youth participants, suggesting that social disconnection is a common experience rather than an isolated concern within the study population. Similar patterns have been documented nationally, where adolescents reporting higher levels ofloneliness also demonstrate increased risk for anxiety, depressive symptoms, and reduced school engagement (Loades et al., 2020; Centers for Disease Control and Prevention [CDC], 2024).
Many respondents in the present study reported limited feelings of belonging and meaningful peer connection, even within school or community settings where social interaction was frequent, reinforcing evidence that the quality of social relationships is more influential than the quantity of social contact (Holt-Lunstad, 2022).
In addition to loneliness, survey data revealed low awareness of available mental health resources, with fewer than half of participants indicating knowledge of how or where to access support. This finding aligns with prior research demonstrating that limited mental health literacy and unclear service pathways are significant barriers to care for adolescents, particularly those from underrepresented communities (Alegría et al., 2018).
Discomfort with help-seeking behaviors was also prevalent, with youth expressing hesitation to seek assistance due to fear of judgment, concerns about confidentiality, and uncertainty regarding adult responsiveness barriers that have been widely associated with stigma and reduced service utilization among adolescents (CDC, 2024).
Qualitative analysis provided critical contextual depth to these findings. Stakeholders consistently described youth experiencing feelings of isolation despite physical proximity to peers, reflecting a disconnect between social presence and emotional connection that has been observed in prior studies of adolescent loneliness (Twenge et al., 2019). Stigma surrounding mental health emerged as a dominant theme, with participants noting that cultural norms, fear of labeling, and perceived social consequences discourage youth from openly discussing emotional distress. These concerns were particularly salient for youth from marginalized backgrounds, where cultural expectations and historical mistrust of formal systems may further inhibit engagement with services (Alegría et al., 2018).
Additionally, stakeholders identified fragmented support systems as a significant contributor to youth social disconnection. Weak coordination among schools, families, community organizations, and mental health providers often resulted in inconsistent follow-up and unclear referral pathways. Such fragmentation has been identified as a structural barrier to effective prevention and early intervention in adolescent mental health (Holt-Lunstad, 2022). When integrated with the quantitative findings, these qualitative themes suggest that youth loneliness is sustained by both individual-level experiences and systemic conditions, underscoring the need for coordinated, culturally responsive, and community-based public health strategies.
Discussion
Discussion Paragraph 1: Youth Loneliness as a Systemic Public Health Issue
Findings from this study indicate that youth loneliness should be understood as a systemic public health concern, shaped by social determinants of health and the organization of support systems rather than as an individual or developmental deficit.
Social disconnection among adolescents is influenced by interacting factors such as socioeconomic conditions, school climate, family stressors, cultural norms, and access to trusted relationships and services (Marmot & Allen, 2020). When these determinants are unfavorable, youth may experience limited opportunities for meaningful social engagement, reduced awareness of mental health resources, and diminished trust in formal systems of care. Prior research has similarly demonstrated that social connection functions as a protective factor for mental and physical health, while its absence is associated with increased risk for anxiety, depression, and academic disengagement (Holt-Lunstad, 2022; Loades et al., 2020).
These findings reinforce the importance of framing youth loneliness as a population-level issue requiring coordinated public health responses rather than isolated, individual-level interventions.
Discussion Paragraph 2: Role of Service Infrastructure and Community-Based
Interventions
The results further suggest that service infrastructure plays a critical role in either mitigating or perpetuating youth loneliness. Fragmented systems characterized by limited coordination among schools, families, community organizations, and mental health providers can leave adolescents without clear or consistent pathways to support. Such fragmentation has been identified as a structural barrier to early identification, prevention, and continuity of care in adolescent mental health (Centers for Disease Control and Prevention [CDC], 2024). Community-based, culturally responsive interventions are therefore essential for addressing social disconnection and promoting youth mental well-being. Programs rooted in community settings, including schools and faith-based or youth-serving organizations, are often better positioned to build trust, reflect cultural values, and reduce stigma associated with help-seeking (Israel et al., 2010).
Culturally responsive approaches that acknowledge youth identities and lived experiences have been shown to improve engagement and reduce inequities in access to care, particularly for underrepresented populations (Alegría et al., 2018). Together, these findings underscore the need for integrated, prevention-oriented public health strategies that prioritize social connection, strengthen community partnerships, and support coordinated service delivery as foundational components of adolescent health promotion.
Tables and Figures
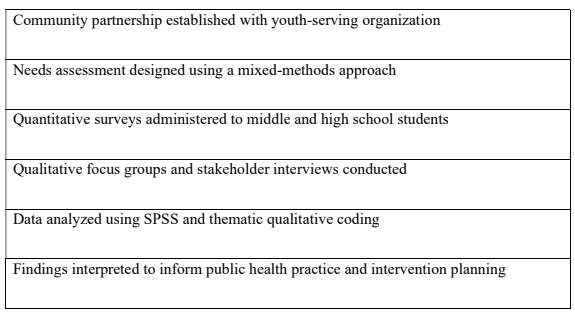
Table 1
Methods Flow Diagram for the Community-Based Mixed-Methods Study
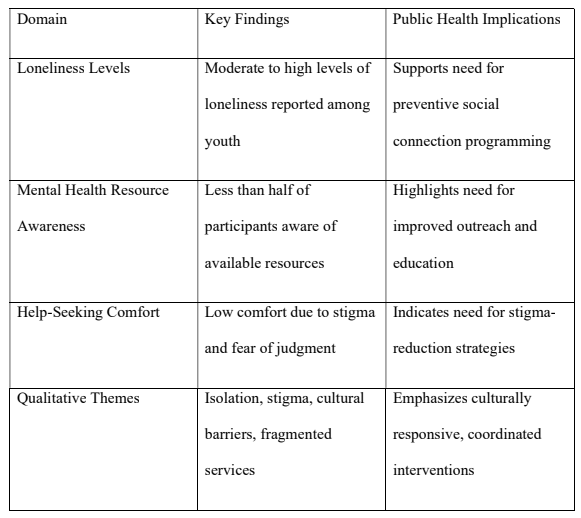
Table 2
Summary of Key Quantitative and Qualitative Findings
Conclusion
Addressing youth loneliness through preventive, community-centered public health strategies represent a critical opportunity to strengthen adolescent resilience, improve mental health outcomes, and promote long-term well-being. Findings from this study reinforce that loneliness among youth is not an isolated or transient experience but a systemic issue shaped by social determinants of health, cultural context, and the organization of support systems (Holt-Lunstad, 2022; Marmot & Allen, 2020). As such, effective responses must move beyond individual-level interventions and instead prioritize relational, environmental, and structural approaches that foster meaningful connection.
Community-based strategies that emphasize early prevention, peer engagement, and culturally responsive support are particularly well positioned to address youth social disconnection. Embedding interventions within trusted settings such as schools, faith- based organizations, and youth-serving community programs can reduce stigma, enhance accessibility, and strengthen engagement among adolescents who may otherwise be reluctant to seek formal mental health services (Israel et al., 2010; Alegría et al., 2018).
Strengthening coordination across education systems, families, and mental health providers further increases the likelihood that youth experiencing early signs of loneliness or emotional distress are identified and supported before challenges escalate (Centers for Disease Control and Prevention [CDC], 2024).
From a public health practice perspective, addressing youth loneliness has implications that extend beyond mental health alone. Social connection is a foundational determinant of health that influences academic engagement, emotional regulation, and long-term health trajectories (Holt-Lunstad, 2022; Loades et al., 2020). Investments in preventive, community-centered approaches therefore have the potential to yield broad and lasting benefits, including reduced mental health disparities and stronger, more connected communities. As concerns about adolescent mental health continue to rise nationally integrating social connection into public health planning and practice is essential for promoting equitable and sustainable youth well-being (CDC, 2024).
References
Alegría, M., Green, J. G., McLaughlin, K. A., & Loder, S. (2018). Disparities in child and adolescent mental health and mental health services in the U.S. The Future of Children, 28(1), 25–47. https://doi.org/10.1353/foc.2018.0002
Centers for Disease Control and Prevention. (2024). Youth mental health: Data and statistics. U.S. Department of Health and Human Services.
Centers for Disease Control and Prevention. (2024). Youth risk behavior surveillance—United States, 2023 (MMWR Supplement, 73[4]). U.S. Department of Health and Human Services.
Creswell, J. W., & Plano Clark, V. L. (2018). Designing and conducting mixed methods research (3rd ed.). SAGE Publications.
Holt-Lunstad, J. (2022). Social connection as a public health issue: The evidence and a systemic framework for prioritizing the “social” in social determinants of health. Annual Review of Public Health, 43, 193–213. https://doi.org/10.1146/annurev-publhealth-052020-110732
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (2010). Methods for community-based participatory research for health (2nd ed.). Jossey-Bass
Loades, M. E., Chatburn, E., Higson-Sweeney, N., Reynolds, S., Shafran, R., Brigden, A., Linney, C., McManus, M. N., Borwick, C., & Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry, 59(11), 1218–1239. https://doi.org/10.1016/j.jaac.2020.05.009
Office of the U.S. Surgeon General. (2023). Our epidemic of loneliness and isolation: The U.S. Surgeon General’s advisory on the healing effects of social connection and community. U.S. Department of Health and Human Services. Palinkas, L. A., Horwitz, S. M., Green, C. A., Wisdom, J. P., Duan, N., & Hoagwood, K. (2011). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health and Mental Health Services Research, 38(1), 44–53. https://doi.org/10.1007/s10488-010-0319-y
Twenge, J. M., & Campbell, W. K. (2018). Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study. Preventive Medicine Reports, 12, 271–283.